Forms
Search & View all MED-Quest forms
Please know that the following applies for all Med-QUEST members statewide:
Are you enrolled in Med-QUEST? Has your contact information changed in the past three years? Please update your contact information with us so you can stay enrolled. Call us at 1-800-316-8005 or log in to your account here to make the change.
We want everyone to Stay Well and Stay Covered.
DHS/Med-QUEST was notified that there were errors to the Chuukese translations on the social media graphics/language located in the toolkit on the Med-QUEST website. We apologize for any confusion these errors have caused. Med-QUEST took quick action to remove the information from the toolkit and the corrected graphics/language will be added in a timely manner.
Our top priority is to improve and sustain wellbeing by providing access to healthcare programs with aloha. Please be assured that we acted swiftly to address the problem once it became known, and that we are actively taking steps to prevent something like this from happening again.
Med-QUEST will be reaching out to members via text messages and phone calls to help them Stay Well and Stay Covered. Text messages will be sent from 45421 and automated phone calls will originate from 808-556-5748. These numbers are only used for outbound communications and no calls will be accepted. If you have questions, please contact the Med-QUEST service center at 1-800-316-8005. Please be aware of scams from other numbers. Med-QUEST will never ask for confidential member financial information over the phone.

Multi-Language Captions
QUEST (Medicaid) Members: Have you moved in the past three years? Don’t miss out on receiving important information regarding your benefits. Call the number on the back of your health insurance card to update your address, phone number, and email today. #medicaid #medquest #staywell #staycovered #healthyhawaii
Multi-Language Captions
If you have QUEST (Medicaid), has your contact information changed in the past three years? Call the number on the back of your health insurance card to update your contact information today. #medicaid #medquest #staywell #staycovered #healthyhawaii
Multi-Language Captions
It’s time to update your contact information for QUEST (Medicaid). Updating your address, phone number and email will ensure you continue to receive important benefits information. Contact your health plan to update your information today. #medicaid #medquest #staywell #staycovered #healthyhawaii
Multi-Language Captions
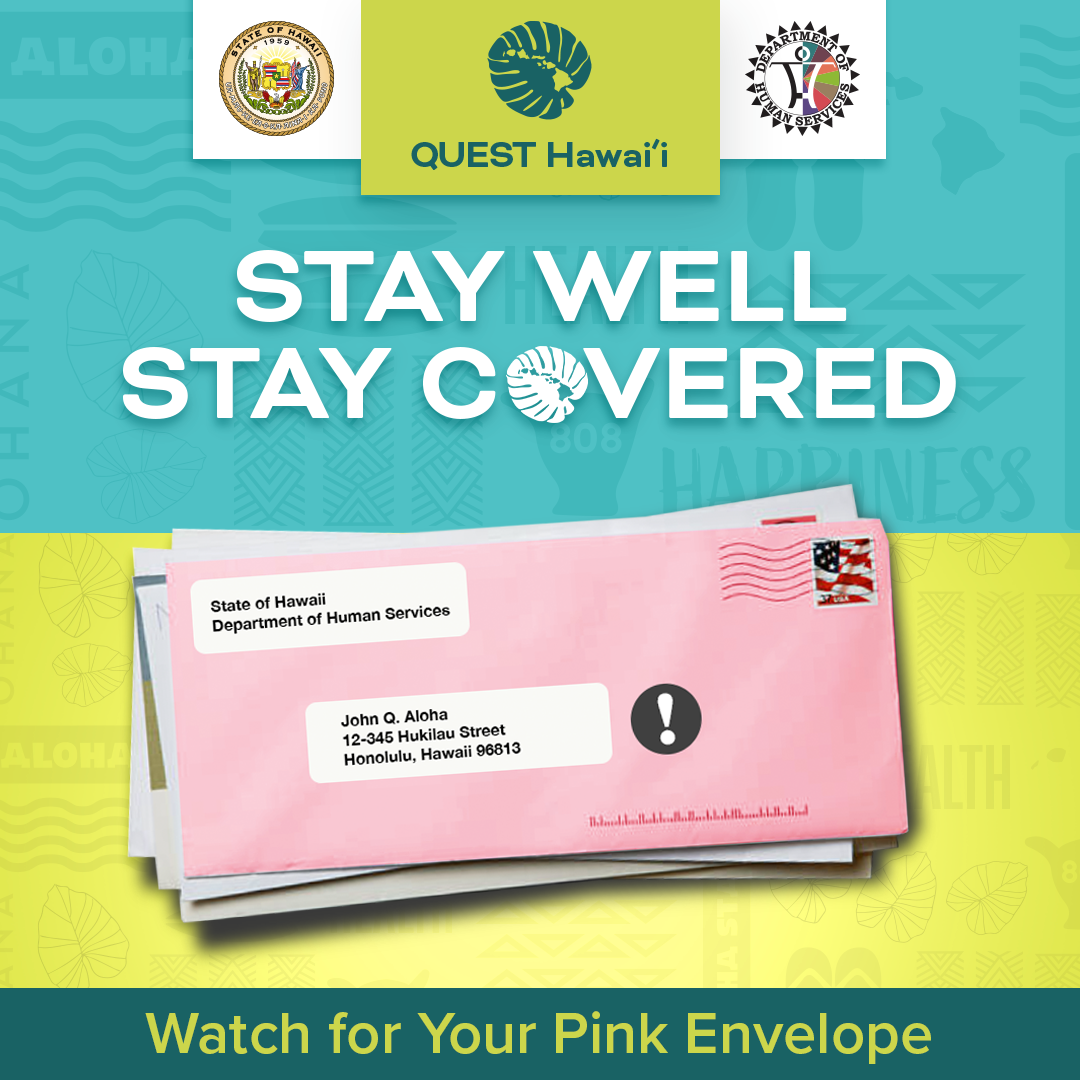
Caption Option #1:
QUEST (Medicaid) members, look for a pink envelope to arrive in your mailboxes within the next year. Stay well and stay covered by following the instructions in the pink envelope for QUEST eligibility renewals. #medicaid #medquest #staywell #staycovered #healthyhawaii
Caption Option #2:
Starting in April 2023 and continuing through next year, QUEST (Medicaid) members in Hawaii will be receiving a pink letter inside a pink envelope from the Department of Human Services. This pink letter will provide members with instructions on eligibility renewals. If you have family who are QUEST members, please be on the lookout for their pink letter and help them stay well and stay covered. #medicaid #medquest #staywell #staycovered #healthyhawaii

Multi-Language Captions
Caption Option #1:
If you need health coverage, but no longer qualify for QUEST (Medicaid), visit the Health Insurance Marketplace at www.HealthCare.Gov or call 1-800-318-2596. There are many options with affordable rates available for those seeking to stay well and stay covered. #medicaid #medquest #staywell #staycovered #healthyhawaii
Caption Option #2:
No longer qualifying for QUEST (Medicaid) shouldn’t be stressful. Visit the Health Insurance Marketplace at www.HealthCare.Gov or call 1-800-318-2596 to find out what your options are for saying well and staying covered. #medicaid #medquest #staywell #staycovered #healthyhawaii

Multi-Language Captions
Caption Option #1:
If you no longer need QUEST (Medicaid) because you have coverage from an employer or another source, please let us know by calling 1-800-316-8005. Letting us know now allows us to help other members to stay well and stay covered in the future. #medicaid #medquest #staywell #staycovered #healthyhawaii
Caption Option #2:
Please call the Department of Human Services at 1-800-316-8005 if you no longer need coverage from QUEST (Medicaid). Help us help other eligible members who need to stay well and stay covered. #medicaid #medquest #staywell #staycovered #healthyhawaii
DHS Forms 1100B-2 (Medical Eligibility Renewal Form) Click here for Renewal Schedule
English
Chinese - Simplified
Chinese - Traditional
Chuukese
Ilokano
Hawaiian
Japanese
Korean
Kosraean
Marshallese
Pohnpeian
Russian
Samoan
Spanish
Tagalog
Thai
Tongan
Ukrainian
Vietnamese
March Newsletter Template - Constituents
March Letter:
Important Information about your Med-QUEST Coverage (Please click on your preferred language below)
English
Chinese - Simplified
Chinese - Traditional
Chuukese
Ilokano
Hawaiian
Japanese
Korean
Kosraean
Marshallese
Pohnpeian
Russian
Samoan
Spanish
Tagalog
Thai
Tongan
Ukrainian
Vietnamese
QUEST Medicaid Coverage Renewal PSA Videos
For Immediate Release
February 15, 2024
MED-QUEST HAWAI‘I LAUNCHES AUTOMATED TELEPHONIC CAMPAIGN
REMINDING MEMBERS TO STAY WELL AND STAY COVERED
HONOLULU – As part of its multi-pronged communications effort, the Department of Human Services Med-QUEST Division (MQD) will launch an automated telephonic campaign this week to remind members about the importance of updating their contact information with the agency. Having members’ correct contact information–including phone number, mailing address, and email address–will help facilitate the coverage renewal process. The telephonic campaign will employ both automated phone calls and SMS text messages.
“Communication with our members is one of our top priorities,” said Medicaid Director, and Med-QUEST Administrator Judy Mohr Peterson. “In addition to the public service announcements in broadcast media and social media, the phone calls and text messages will provide yet one more avenue to reach members to help keep them covered.”
Med-QUEST will send telephonic messages to members prior to and shortly after their coverage renewal dates. Automated phone calls will be sent through a dedicated phone number, 808-556-5748. SMS text messages will be sent through a dedicated SMS short code, 45421. These numbers are only being used to facilitate outbound communications and will not accept inbound calls or texts from members. If members have questions, they are encouraged to call Med-QUEST at 1-800-316-8005.
Med-QUEST reminds the public that it will never ask for members’ financial information via text.
Med-QUEST reminds members who have yet to be contacted to do the following to prepare for their renewals:
During the renewal process, some people may no longer be eligible for coverage through Med-QUEST. If a person is determined to no longer be eligible for coverage, we encourage them to check with their employer to see if they qualify for employer-sponsored coverage.
If a previous Med-QUEST enrollee is not eligible for health insurance through their employer, they should please visit the Health Insurance Marketplace at HealthCare.Gov or by calling
1-800-318-2596 to make sure they stay well and stay covered!
###
Media Contact:
Amanda Stevens
[email protected]
Public Information Officer
Department of Human Services
----------
For Immediate Release
February 16, 2023
HONOLULU – Throughout the pandemic, all Medicaid members received continuous uninterrupted coverage amid the public health emergency. Med-QUEST Division (MQD) under the Department of Human Services, will begin reaching out to members in March to let them know what month their eligibility will be redetermined. This eligibility renewal work will begin in April and be spread out across 12 months.
MQD wants to assure people that their Medicaid coverage will remain active until their case is up for renewal. We anticipate that most current members will continue to be eligible for coverage, but for those who may no longer be eligible, our MQD staff will help connect them with affordable coverage on the HealthCare.Gov Marketplace. Or, if Medicaid coverage is no longer needed, please contact us and let us know.
Members will receive a pink letter that contains eligibility renewal information one month prior to their month of renewal. This means that renewal notices will go out as early as April 2023 (for May 2023 renewals) and as late as March 2024 (for April 2024 renewals).
Please note that this notification process will happen over a one-year period. This means that not all Members will receive their pink letters at the same time. A plain white letter will be sent in March to every Med-QUEST household letting them know the month of their scheduled redetermination. The redetermination months will range from May 2023 to April 2024.
In preparation for this renewal period, Med-QUEST asks members to do the following:
“We emphasize to members that it is very important to update their contact information with their health plan and encourage them to respond to all Med-QUEST/Medicaid communication in a timely manner to ensure continuous coverage,” said Judy Mohr Peterson, Medicaid Director, and Med-QUEST Administrator.
Before mailing a renewal notice, Med-QUEST first seeks to renew its members eligibility using available and approved data. Only if MQD cannot renew a member’s coverage using these data sources, will the member be asked to provide additional information listed within the pink letter. For those members whose cases MQD can renew without needing additional information, the pink notice will contain a confirmation of renewed coverage and no further action will be needed at that time.
To access the Frequently Asked Questions document, click here.
Media Contact:
Amanda Stevens
[email protected]
Public Information Officer
Department of Human Services
About Med-QUEST/Medicaid: The Department of Human Services is the state agency designated to administer Medicaid, a program jointly funded by federal-state funds that provides health care coverage and other benefits to eligible individuals. These include children, pregnant women, parents of eligible children, adults, children in foster care and young adults previously in foster care, aged, blind or disabled, and those in nursing homes.
COVID-19 Impacts: Since the beginning of the COVID-19 pandemic, there have been more than 138 thousand new enrollees who receive Medicaid coverage, a 42% increase since March 6, 2020. With total enrollment now at more than 465,000, Medicaid covers 1/3 of Hawaii residents and includes more than half of Hawaii’s keiki. Enrollment is at a historic high due in part to the continuous coverage provisions allowed during the public health emergency. During this public health emergency, no one was disenrolled unless the member moved out-of-state, requested that their coverage be terminated, or the member died.
For downloadable FAQs in various languages, please click below links.
At the beginning of the COVID-19 pandemic, the federal government declared a public health emergency (PHE). During the PHE, Medicaid agencies like QUEST Integration (Hawai`i’s Medicaid program) did not disenroll members, even if someone’s eligibility changed. In December 2022, Congress passed legislation which decoupled the Medicaid continuous coverage requirement from the COVID-19 PHE and instead directed that the continuous coverage requirement would end on March 31, 2023, regardless of the PHE dates.
The notification process will happen over a one-year period starting in April, 2023 and ending in March, 2024. Because of the sheer number of current members–over 465,000+ to date–not all Members will receive notification at the same time. Member renewals have been divided evenly across the 12-month period.
In preparation for this renewal period, Med-QUEST asks members to do the following:
One month prior to their month of renewal, members will be mailed a pink envelope with a pink letter that will contain eligibility instructions. Starting in April, we will begin reviewing cases with a May renewal date. If those members with May renewal dates are no longer eligible, their coverage may end as early as June 1, 2023.
With very few exceptions, MQD will renew an entire household at the same time.
In most cases, yes, unless you have moved, and your current health plan is not available in your new location.
A member who is no longer eligible, will receive:
We have already started a mass media campaign, including ads in movie theaters. Television and radio public service announcements will follow. We will utilize earned media opportunities and inclusion in community partner and legislative constituent communications. In addition, we intend to reach out to each QUEST member with a plain white letter in March to inform them of the process and let them know which month their case will be up for renewal.
Our STAY WELL STAY COVERED communications campaign toolkit on the Med-QUEST website will include messaging via printed and out-of-house channels, such as newspapers and banners. The renewal notification will be mailed, so members without internet access will still be able to receive the information.
We will initiate the last batch of eligibility renewals in March, 2024 for cases up for renewal in April, 2024. For some individual cases, verification may take up to 60 days to complete, so the final verifications for all members should be completed by the end of May, 2024.
This information was developed with contributions from the State Maternal Health Innovation Program, a program supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $1 million per year for five years, subject to availability of funds, with zero percent financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.